In October 2012 Dr. Santorino Data took the microphone and made a 60 second pitch to a group of engineers, designers, clinicians and entrepreneurs who gathered at the CAMTech H@cking Medicine Hackathon at Massachusetts General Hospital. It was not an elevator pitch in the traditional sense, but holding a conventional bag valve mask (BVM) resuscitator, Dr. Data described its use in training. He distilled his vast experience with neonatal resuscitation and training frontline care providers into a problem statement: despite improvements to and increasing availability of training and equipment, many infants still die preventable deaths due to breathing problems. Trainees successfully complete training, yet often fail to provide adequate ventilation in the field.
Dr. Data asked for some way to passively log time and date-stamped data to objectively audit care providers and the root cause of newborn death related to breathing trouble at birth. Why did this baby die? Was the provider’s technique timely and correct? Had their skills atrophied since initial training? Was the resuscitation equipment functioning properly? Was this baby simply (and tragically) too sick to save?
It is a rare thing to have an expert like Dr. Santorino Data in the room. Leaders within the American Academy of Pediatrics (AAP) have stated that Dr.Data has trained the most people in the Helping Babies Breathe program globally. This vast experience gave him insight into the challenge of preventing newborn deaths and complications due to breathing problems.
After his pitch, and many other compelling pitches from other clinicians, entrepreneurs and engineers, teams formed to work on the ideas, or generate new ones for successive rounds of pitching, ideation, and prototyping.
Dr. Data’s problem attracted two engineers none of whom had met before the event. Dr. Data also attracted the interest of an MGH clinician-educator Dr. Kristian Olson.

Craig, Kevin and Data working at the original hackathon.
The engineers included Craig Mielcarz, a freelance electrical engineer with a strong background in prototype development of consumer electronic and medical devices and Kevin Cedrone, then a mechanical engineering PhD student studying automotive engine combustion. To Kevin, the problem of measuring and diagnosing ventilation quality resembled the a similar and routine task he faced in the engine lab. In what may be considered a callous engineering analysis, the inhalation and exhalation of a newborn struggling to breathe has much in common with an engine that aspirates a fuel-air mixture and expels hot post-combustion exhaust. Armed with MIT education, and free coffee at the Hackathon, Kevin and Craig went on to flesh out their mental model infant resuscitation: how it should work, and what typically goes wrong when it does not work. The main problems of ventilation, as one may guess, or find out from experts like Dr. Data and Dr. Olson are:
1. Poor seal between the bag-valve-mask interface
2. Blockage in the airway (due to secretions, poor airway alignment, etc.)
3. Incorrect rate of ventilation (usually too fast)
4. Insufficient volume and/or pressure to inflate the lungs
Kevin and Craig proposed a simple, low-cost device that could be added to the flow path of existing BVM equipment to observe the quality of ventilation technique. Before building such a device, the team pivoted. Rather than simply record ventilation efforts for literal post-mortem analysis, the same device could, with very little modification, provide real-time feedback during resuscitation. Instead of waiting for the worst possible outcome, the death of a newborn, to trigger corrective action like bringing a birth attendant in for retraining, or finding and fixing faulty equipment, why not give live guidance, exactly when it matters most?
That evening, the engineers hatched a scheme to build a proof-of-concept prototype. Overnight, Craig and Kevin combined ventilation tubing from MGH, some sensors Kevin had saved from the trash can in the Sloan Automotive Laboratory at MIT, and an Arduino with a custom algorithm. Two low-cost measurements were enough to make a high-value judgment about the quality of ventilation.
With a working prototype, the team pivoted again. The team recognized another potential market and purpose of the device. Why wait until an emergency intervention to give feedback to caregivers? Why not make this device available during training. Give trainees objective feedback on their technique as early as possible, and as often as possible. Give trainees a device to take with them so they can continue to practice when the stakes are low, so they are ready and able to give the highest quality ventilation in as timely a manner as possible.
The team presented their hack to a panel of judges and won first prize for best prototype and best overall innovation, including a demo of the ugly but fully functional proof-of-concept prototype.
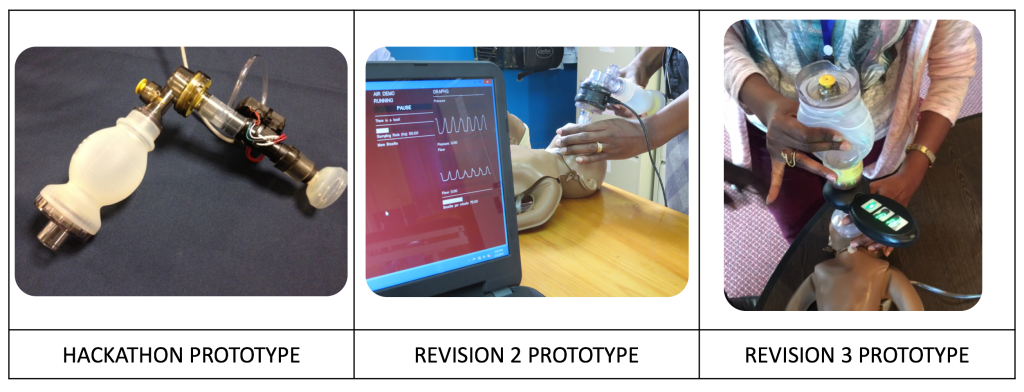
The original proof of concept prototype installed in the air path of a Laerdal bag valve mask.